The following is an excerpt of a guest column by Helio Fred Garcia published by CommPro.biz on July 10, 2023.
Judge Terry A. Doughty’s ruling enjoining federal government departments and employees from urging or even encouraging social media platforms to remove false and dangerous information is an affront to justice, to democracy, and to truth. It is not only suppression of the very freedom of speech the judge claims to be upholding; it prevents government departments from exercising their duty to keep people safe.
Disinformation and misinformation kill, both people and democracy.
Nine months into the COVID pandemic, Cornell University’s Alliance for Science warned that “if people are misled by unscientific and unsubstantiated claims about the disease, they may attempt harmful cures or be less likely to observe official guidance and thus risk spreading the virus.”
In a joint statement with global public health organizations, The World Health Organization warned of the dangers of disseminating false or misleading information about COVID:
“Misinformation costs lives. Without the appropriate trust and correct information, diagnostic tests go unused, immunization campaigns (or campaigns to promote effective vaccines) will not meet their targets, and the virus will continue to thrive.”
In 2021, disinformation and misinformation about the COVID vaccine, fueled by conspiracy theories, persuaded millions of Americans to refuse to be vaccinated against COVID. In a ten-month period after the vaccine became universally available at no cost in the United States, more than 250 thousand Americans who had refused to be vaccinated died. This led the head of the United States Food and Drug Administration one year ago to warn that misinformation had become the leading cause of death in the United States.
Judge Doughty is the same judge who blocked the Biden Administration’s mandate that healthcare workers be vaccinated. That suit was brought by some of the same plaintiffs who are trying to prevent public health officials from meeting with social media platforms.
His ruling this week is ideology masquerading as jurisprudence. He conflates good faith attempts to protect public health and save lives with suppression of “conservative speech.”
Disinformation is a signal threat to public health, civic order, and democracy. Much disinformation on social media platforms is planted by or intensified by the nation’s strategic adversaries.
And disinformation is a signal opportunity for professional communicators to do what we do best: to shape public opinion and to resist those who will use disinformation and misinformation in ways that cause great harm.
We who communicate in, for, and about businesses have a particular obligation to detect disinformation, to call it out, and to avoid spreading it further.
Judge Doughty ends his 155-page Memorandum Ruling by arguing that the “United States Government seems to have assumed a role similar to an Orwellian ‘Ministry of Truth.’”
That statement itself is disinformation. It is also – how can I put this? – Orwellian.

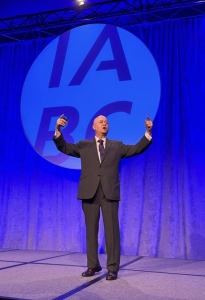 Garcia examined the ways in which disinformation and misinformation can – and have – put human life and democracy at risk. He then outlined a disinformation playbook that, once known, can be used to stop the spread of disinformation.
Garcia examined the ways in which disinformation and misinformation can – and have – put human life and democracy at risk. He then outlined a disinformation playbook that, once known, can be used to stop the spread of disinformation.